The evolution of supramarginal tumor resection in to supra‑complete surgery according to the DiVA protocol.
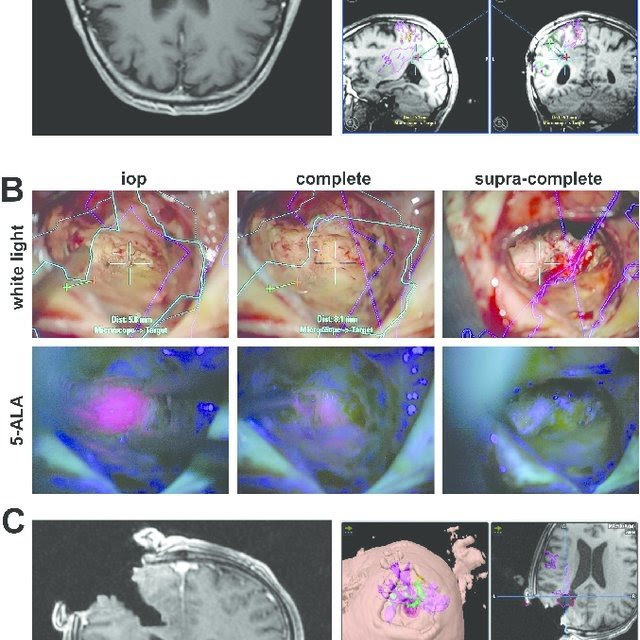
(A) the T1‑weighted MR‑scans show a contrast agent enhancing space occupying lesion at the occipital horn on the left side (left image). The tumor was preoperatively segmented and the data sent to the neuronavigation (right image series).
(B) white light microscopy is depicted in the upper row and 5‑ALA fluorescence microscopy in the lower row. The left column depicts the point in surgery following resection of the primary tumor bulk, represented by a distinct 5‑ALA signal. Following resection of the tumor bulk, vague 5‑ALA fluorescence can be identified in the depth of the resection cavity (middle column). Conventional glioma surgery would entail ending the surgery at this point. Supramarginal resection would entail additional, unspecific peritumoral resection. In contrast, supra‑complete surgery as a further refinement to conventional supramarginal resection entails selective resection of the vague 5‑ALA fluorescence positive areas until no signal is detected any longer (right column).
(C) the intraoperative T1‑weighted MR‑scan with contrast agent administration confirms the planned extent of resection (left image); there is no pathological contrast agent enhancement detectable any longer. Superimposition of these intraoperative images with the original segmentation demonstrates resection beyond the contrast agent enhancing areas in terms of a tailored supramarginal resection (right image series).