Meningioma | Dr. Prem Pillay, Singapore
The Meningioma is a primary intracranial tumor that is one of the most common benign tumors within the cranium (head). About 40-60% of benign tumors are meningiomas. About 15% of all primary intracranial tumors (both benign and malignant) are meningiomas. Origin: They originate from the archnoid cap cells that occur most often at the arachnoid granulations which are near the midline adjacent to the superior sagittal sinus (the large midline vein of the head). Another location is the tela choroidea in the ventricles. They are therefore intracranial but not intracerebral (within the head but not in the brain). In other words they occur usually from the covering of the brain called the dura and not from within the brain.
| Age: | The peak age is from a 40 to 60 years. |
| Sex: | It is more common in females than males |
| Genetics: | 72% of tumors have monosomy 22. |
| Risk factors: | Previous radiation, neurofibromatosis type 2 (NF 2). |
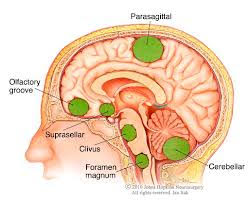
| Locations: | Cranial (within the head): 90%, spinal canal : 9% and others 1% (neck, parotid etc) About 50% are parasagittal and convexity (near the midline and over the lobes of the brain). |
| Grading: | WHO classification I,II,III from that least to the most aggressive. |
| Pathology: | Meningothelial, fibroblastic,psmmomatous, angiomatous, and transitional (most common). |
| Aggressive variants: | they invade brain, have necrosis, mitosis, papillary, or are locally recurrent. |
| Malignant: | As above with metastases. |
| Clinical Features: | They either be symptomatic or asymptomatic at the time of discovery. The usual symptoms may include headaches, seizures, loss of any of the senses (smell, taste, hearing, vision, sensation) , motor weakness (hemiparesis ), memory loss, language problems (dysphasia, aphasia) . Some people with these tumors are mistakenly diagneosed with Dementia , strokes or psychiatric problems. |
| Diagnostic tests: | This includes a thorough neurological examination followed by brain scanning. In an emergency situation a CT of the brain with contrast can be done quickly, but an MRI of the brain with gadolinium is still the definitive test.
The appearance of a meningioma on these tests is usally unique or characteristic enough for an accurate diagnosis most of the time. There are exceptions where a biopsy with tissue examination is still needed. |
Biopsy
A biopsy is not mandatory for the diagnosis of a meningioma. MRI and even CT of the brain can be fairly clear in determining the diagnosis of a meningioma. The presence of an intracranial but extracerebral enhancing tumor with a dural tail is a classical finding.
A biopsy can be done by the technique of stereotactic computer aided biopsy where a needle is guided to the tumor after detailed computer planning is done based on pre-surgical imaging and using a stereotactic frame. There is also the technique of frameless stereotaxis using a system like the SteathStation.
Surgery
Microsurgery using a high definition microscope and microinstruments is the latest type of surgery for meningiomas. CAN/CAM technology can also be used. Lasers,”Super-Lasers”,CUSAs and the Malis technique can be used for tumor removal. The StealthStation and other neuro-navigation systems are useful in allowing a minimally invasive approach in the removal of these tumors.
Radiosurgery
Radiosurgery refers to computer planned, and accurately focused high energy beams that are used for non-invasive tumor treatment. Radiosurgery has been shown to be effective for the treatment of meningiomas. Modern systems in use include the Gamma-knife, Novalis type systems and the latest system of Tomotherapy. The two ways in which the treatments can be given are either in a single session or in multiple sessions. The latter is often referred to as SRT (stereotactic radiation therapy) or FSR (fractionated stereotactic radiosurgery). New forms include MicroRadiosurgery and Proton Beam Therapy.
Medications
There are few anti-meningioma medications. They are only mildly effective at best.
Combined treatment
Combined Microsurgery and Radiosurgery (CMR) is where both modalities are used for the treatment of large , difficult to remove, or dangerous location meningiomas. This can be a lower risk protocol for complete tumor removal especially in higher risk patients.